A multi-disciplinary team led by Trinity researchers has found a potential new therapeutic target for treating degeneration of the retinas.
The team discovered that a protein involved in injury to nerve cells may also have a role in the progression of retinal degeneration.
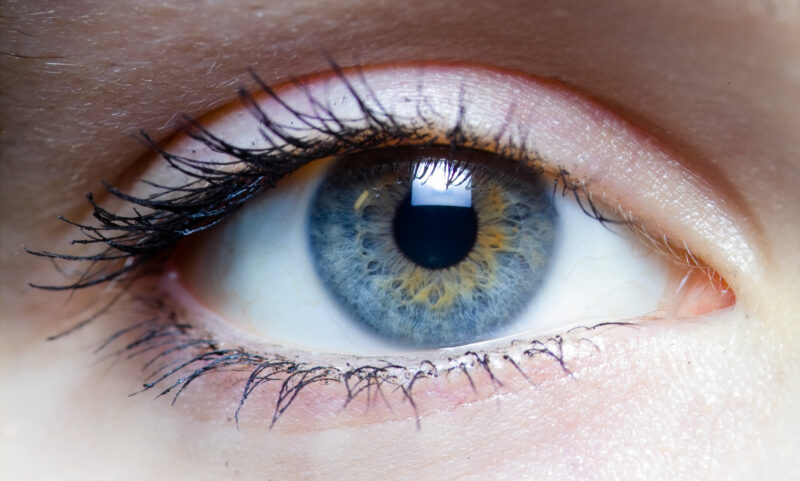
Millions of people worldwide suffer from varying degrees of vision loss due to diseases which cause irreversible damage to the retinas of the eyes.
In Ireland, approximately 5,000 people are affected by inherited retinal degenerations, while another 80,000 are known to live with age-related macular degeneration, which also affects the retinas.
In a press statement, Dr Ema Ozaki, a research fellow in clinical medicine at Trinity, said: “Lots of different factors can initiate retinal degeneration and lead to severe visual impairment and eventual blindness, but ultimately the end-point is photoreceptor cell death. Although it seems unlikely the process of cell-death is – in fact – a programmed or organised event that directs proteins in our cells to take on ‘executioner’ roles.”
Photoreceptor cells are specialised neurons found in the back of the eyes that convert light into electrical signals that facilitate sight. Retinal degeneration leads to the death of these photoreceptor cells.
The research team, led by Dr Sarah Doyle, an assistant professor in immunology at Trinity, investigated one such “executioner protein”, SARM1.
This protein has come to light recently in brain and spinal injury research as it triggers the degeneration of nerve cells. SARM1 has come to the fore recently in the study of brain and spinal injury, as it is highly efficient at triggering the degeneration of neuronal cells. While the retina is an extension of the brain, this report is the first to describe a role for SARM1 in photoreceptor cell biology.
Explaining the significance of this research, the first to study SARM1 in terms of retinal degeneration, Dr Sarah Doyle, said in a press statement: “Our research indicates that SARM1 is likely to be a key executioner in the process of retinal degeneration, because if we remove it from our experimental model system this has the effect of delaying the photoreceptor cells from dying.”
Doyle continued: “This is an important finding because the first steps involved in processing ‘light into sight’ take place in the photoreceptors. As a result, losing photoreceptors ultimately equates to losing vision.”
“For this reason”, she said, “interventions that prevent or delay photoreceptor cell death are critical to preserve sight for as long as possible in people with degenerative retinal diseases”.
The research team was also able to show that the protected and surviving photoreceptors maintained their function, thus enlightening the therapeutic potentials of targeting the SARM1 protein.
Doyle added: “This is particularly exciting for the future because others have recently shown that a gene therapy approach for inhibiting SARM1 is effective in protecting against neuronal degeneration. We know that gene therapy is well suited as a treatment for retinal disease, so such an approach for inhibiting SARM1 activity may offer an option for protecting vision across multiple retinal degenerative diseases.”
The research involved experts from Trinity’s Schools of Medicine, Biochemistry and Immunology, Genetics and Microbiology, and Engineering and was funded by HRB-MRCG (Fighting Blindness), Science Foundation Ireland, the Irish Research Council, the NCRC, and BrightFocus Foundation.