Ralph Hurley O’Dwyer | Contributing Writer
Eradicating cancer has been the Holy Grail of medical research for the last fifty years. Many a scientist or medic has dreamed of stumbling upon a magic pill or potion which would cure cancer and the suffering it creates. Perhaps the closest candidate to such a “magic bullet” today is the human papillomavirus vaccine, often termed the “cervical cancer” vaccine. In fact, the colloquial name given to this vaccine betrays an unfortunate yet widespread misconception. Most Irish people believe that the HPV vaccine benefits solely women, with protection against cervical cancer its only merit. However, the HPV vaccine can prevent a plethora of different cancers in both men and women, both cheaply and effectively. For a complex variety of reasons, the HSE has failed to take account of this truth in their national, female-only vaccination program in schools, resulting in a discriminatory policy which unfairly threatens the wellbeing of Irish men and women.
What is the HPV virus?
HPV (human papilloma virus) is a common virus contracted almost ubiquitously by humans. A variety of subtypes exists, some of which cause common warts, others which cause genital warts and certain cancers , principally cervical cancer as well as anal, throat and penile cancers. Over 90% people will contract common warts at some stage in life, with over 80% sexually active individuals contracting at least one genital strain of HPV by the age of 50. Most people contract genital HPV in the first two years following the onset of sexual activity. It is important to take note that condoms do not protect fully against HPV infection.
HPV infections in most people are cleared rapidly by the immune system. However when initial HPV infections do not clear, HPV causes damage to cellular DNA, often leading to uncontrolled dividing cells – cancer.
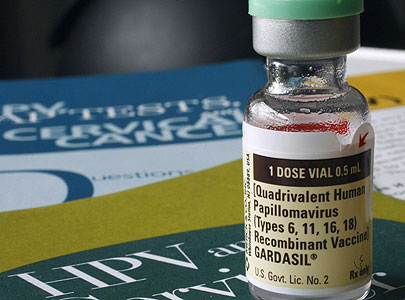
Two HPV vaccines exist currently on the market. Cervarix protects against the carcinogenic subtypes 16 and 18. Gardasil, the HPV vaccine currently administered free of charge to girls in 1st year of Irish secondary school, provides immunity against four strains of the HPV virus: the carcinogenic strains 16 and 18 in addition to strains 6 and 11, which account for more than 90% of genital warts.
Why aren’t boys currently vaccinated as well?
The current reasoning behind female-only HPV vaccination is founded on the fact that cervical cancer, affecting only women, is the most common of the HPV-associated cancers. Moreover, although males can still contract genital warts and carcinogenic sexually-acquired HPV strains, it is argued that since most men have sex with women of the same age, they will be protected against these strains, most of their partners being vaccinated and thus free of infection. A number of flaws exist with this reasoning however.
Firstly, Irish males are not having sex in a geographically and age-restricted bubble. The free public Gardasil vaccination scheme in Ireland was only introduced in 2012 for the Leaving Cert class of that year. Thus any girl, aged 20-21 and over, will not have been vaccinated and thus may contract the virus and pass it on to younger men in the future. Moreover, these younger men may in turn infect uninfected older women. Furthermore, most countries have no public HPV vaccination policy. This includes not only most developing countries but also seven EU member states such as Finland and Poland. The Irish government may like to think they are protecting males in secondary school today by vaccinating their female classmates. In an ever more mobile world however, it is naïve to expect these men to limit their sexual pool to Irish females a maximum of two years older than themselves.
According to a TCD study in St. James’s Hospital, published in June, 70% of MSM (men who have sex with men) test positive for carcinogenic HPV strains.
Secondly and perhaps most importantly, it is naïve to expect all males to limit their sexual partners to solely other females. MSM(men who have sex with men) benefit from no herd immunity and are thus at extremely high risk of contracting the HPV virus and consequently a myriad of possible health problems, ranging from anogenital warts to lethal penile, anal and throat cancers. According to a TCD study in St. James’s Hospital, published in June, 70% of MSM test positive for carcinogenic HPV strains.
The cost benefits of vaccinating future MSM is demonstrably clear. However in practise selecting this population is difficult. Asking a classroom of 12 year old boys to raise their hand if they plan on having sex some day later with another male, in order to determine whether they should receive the HPV vaccine, is laughable in its infeasability . Considering that most individuals acquire HPV in the initial year or two after commencing sexual activity, ensuring vaccination of MSM would rely on targeting males somewhere between coming out and becoming sexually active, events which frequently occur in the opposite direction. Relying on gay teenagers to present themselves at their GP the moment they realise or accept they are something other than fully heterosexual is fraught with problems. Few teenagers have €500 at their immediate disposal to cover the costs of vaccination. This effectively forces teenagers to beg for a substantial sum of money to guarantee their future health. “Hey Dad. Could you give me 500 euro? I need it because I fancy having anal and oral sex with men in a few years’ time.” Finding the courage to consult one’s GP regarding one’s sexual health can be difficult enough, without the additional burden of coming out simultaneously and coming up with 500 euro. Furthermore, obtaining HPV vaccination is compounded by the fact that most GPs are unaware that Gardasil is now approved for use in males.
However, anal, penile and oropharyngeal cancers do not occur solely in MSM. The publicity surrounding the ostensibly straight Michael Douglas’s disclosure of his HPV-acquired throat cancer illustrates just one such example. Rates of HPV-related oropharyngeal cancer in particular are soaring amongst non-MSM, perhaps due to the increasing popularity of male-to-female oral sex. According to Scandinavian epidemiological studies, the prevalence of oropharyngeal cancers has increased more than eight times since 1994 amongst men under 40, the majority of this increase attributable to non-MSM.
In 2012, Australia became the first country in the world to implement a gender-neutral, universal HPV vaccination program in schools. Austria soon followed suit. Male vaccination is also recommended by the Centres for Disease Control(CDC) in the USA and the Canadian National Advisory Committee on Immunization. In the UK, there already exists a growing trend for more informed and affluent parents to vaccinate their sons privately, thus exacerbating already existing inequalities in cancer prevention and treatment. Considering that the multi-course series of injections necessary to ensure immunity costs approximately €500 privately, unfortunately vaccination remains an unaffordable option for many parents.
In essence, the reluctance of our government and health service to properly consider this issue is rooted in an ingrained shame of sex.
Although HPV vaccination is most effective if undertaken before sexual debut, data from a recent TCD study has illustrated that vaccination is still effective in certain high-risk populations, even a number of years post commencing sexual activity. Amazingly, the Irish National Immunisation Programme rejected a request for HPV vaccine funding in the spring for an unspecified gay men’s health clinic. This is despite the fact that the 2013 Immunisation Guidelines for Ireland stated the vaccine should be offered to MSM.
In essence, the reluctance of our government and health service to properly consider this issue is rooted in an ingrained shame of sex. Establishing a HPV vaccine programs for girls upset our Catholic sensibilities enough considering it is contracted predominantly through heterosexual vaginal sex. Widening the immunization programme to prevent men developing cancer caused predominantly through homosexual oral and anal sex evidently stretches the HSE’s sensibilities one step too far. Unfortunately, in the view of many, these are dirty cancers caused by dirty people doing dirty things. We’d rather pretend such illnesses didn’t exist.
Furthermore, the HSE’s vaccination program propagates the false belief that females alone are responsible for contracting and propagating STIs, conveniently ignoring the primary mode of HPV transmission to women, namely – sexual contact with men. Whether unconsciously or not, this policy mirrors Irish attitudes to pregnancy in the past, where women were deemed solely responsible for becoming pregnant. Indeed uptake of the HPV vaccine amongst girls in the UK has been very low among certain religious minorities, the belief being that women don’t require vaccination if they are monogamous, wholly ignoring the sexual behaviour of men. Low uptake among such groups poses a major risk to both men and women.
That such a flawed and discriminatory program is tied to the education system, heightens its injustice. By vaccinating only girls, our educational system signals to students that women alone are responsible for HPV and that men are devoid of responsibility for its contraction or propagation. Furthermore, it signals to gay or bisexual male students in particular, that their health is valued less than their straight classmates.
Ireland has an opportunity to rectify an injustice and join a group of world leaders in public health and equality. It is time that our health system based its decisions on necessity and reason, not on embarrassment or sexual shame.
There is no valid scientific argument against sex-neutral HPV vaccination. Financial concerns remain the only logical constraint to be considered. To date, the HSE has not considered extending vaccination to males to be cost effective. However, a number of flaws exist with the cost analysis studies performed. Furthermore, while currently administered in three doses, new research indicates that two or perhaps even one dose of the vaccine may be sufficient to ensure immunity. This new finding could thus reduce by one half or one third the price of vaccination. HPV Action, a UK-based collaboration of 33 professional medical and patient organisations, including the British Dental Association, the Royal College of Obstetrics and Gynaecology and The Royal Society for Public Health, has suggested that a student may be immunised for only £45, citing figures from Scandinavian analyses.
Ireland has an opportunity to rectify an injustice and join a group of world leaders in public health and equality. It is time that our health system based its decisions on necessity and reason, not on embarrassment or sexual shame. No longer can we justify the suffering and heartbreak of the many men who die every year from easily-preventable HPV-related cancers. A gender-neutral virus requires a gender-neutral vaccination programme.